Topic:
Resource type:
Authors:
Publication date:
Date added to Learning for Involvement:
Supporting equity and tackling inequality: how can NIHR promote inclusion in public partnerships?
An agenda for action
Candace Imison, Meerat Kaur, Shoba Dawson
Contents
Foreword
Much of my personal experience in forming a view about inclusion, particularly in health research and involving the public in the debate, has been based on my family, particularly as my first generation ‘Windrush’ parents became older and more dependent on healthcare services.
They were totally bemused with the language and terminology, thinking they were not educated or articulate enough to be engaged. I have a strong memory of my father looking helplessly at me when 2 health practitioners were talking over him about the design of a healthcare package. Yet, my parents were political animals, passionate about the development of their children and grandchildren, and they read everything there was to read about civic and social duties.
Why were they so afraid or uninterested in health research? I now realise it was because no-one asked them about their experiences or views in the culture and language of their heritage. I have since discovered this to be true of other minority groups who in the main are the most disadvantaged.
This Agenda for Action must be seen as a long-term process and not a quick fix in developing a relationship with diverse and dynamic communities that have enriched and contributed to our nation.
Angela Ruddock – Public Contributor – Project & Research Team
When we started on this review, I worried about what we could actually positively achieve as the agenda is huge and complex. However, the subject is much too important and growing in urgency to put back into the ‘too difficult to do’ box, as it often is. Further into the project, when engaging with a wider group of public contributors, they too sighed. We’ve all been here so many times before, yet without satisfactory resolution.
I was once helped in my thinking by another long-term service user. They said that we should learn to celebrate diversity, to be aware of our own prejudices, and shouldn’t see difference as a threat. We should indeed be positive about our difference. In trying to tackle health inequalities, we need to form public partnerships in research with the very people we ought to be helping the most. Co-produced research leads to better understanding and appropriate health and care response. The time is now…
Tina Coldham – Public Contributor – Project & Research Team
Executive Summary
“Culture change is at the heart of this. Otherwise we are involving underserved communities in an environment that isn’t fit for purpose. We need to explicitly acknowledge the things that are challenging, including research hierarchies, in order for anything to change.”
Lynn Laidlaw, Public Contributor, Steering Group Member
This report sets out an Agenda for Action within the NIHR and the research it funds and supports. The Agenda aims to promote health equity and reduce health inequalities through greater inclusion in public partnerships. This narrative Review is based on a range of evidence, including published studies, stakeholder feedback and grey literature. A steering group with relevant academic and lived experience expertise guided the Review and helped generate actionable insights.
The term public partnerships describes ways in which patients, service users, carers and members of the public work with researchers, and health and care professionals, in the creation and use of health and care research. This includes all activities in involvement, participation and engagement. Inclusive partnerships need to recognise the constellation of factors that give each of us our unique perspective, based on our experience of discrimination and privilege. These unique perspectives should be seen as assets, and opportunities to strengthen health and care research.
The NIHR aims for equality in involvement, engagement and participation in the research it funds and supports. Despite some excellent practice, the NIHR recognises that this ambition is yet to be achieved. This review heard widespread frustration at the lack of progress. There are systemic challenges facing the research and wider community in achieving that ambition. A long history of exclusion in society has left a legacy of deep-seated health inequalities. Exclusion from society has also led to the lack of inclusion in research and practice, which further increases health inequalities. This then reinforces the disadvantage embedded in wider society and culture. We need to break the cycle of exclusion and inequality.
To do this, the relationship between research institutions, researchers and communities needs to change. We should not expect the public to fit into research systems. Instead, we need to help researchers get closer to communities. We need to give communities the platform and power to influence and initiate research. We need to address the current mistrust of research and researchers, and replace it with trust. This is not only about race but all marginalised and underserved communities.
The NIHR has opportunities to strengthen inclusion and diversity across the research cycle. To change the culture and ways of working, four related issues need to be addressed.
- Resources – the time and money to overcome barriers to engagement and support inclusive partnerships.
- Partnership skills – to help research teams, university staff, health professionals and engagement leads engender trust and develop reciprocal relationships with communities, respecting and valuing different knowledge bases.
- Wider incentives – to create inclusive partnerships. For example, funders’ expectations of research teams and wider criteria for academic success and progression. These need to foster a diverse research workforce as well as inclusive research approaches
- Personal motivation – reinforced by all the above, to engage, share power and create a meaningful partnership.
The Review has identified notable examples of good practice within and outside of NIHR (see Appendix C). Many researchers are already working with communities, and building trusting relationships in collaborative partnerships that empower people. Drawing on evidence from the literature alongside stakeholder feedback and a systematic analysis of the NIHR’s current activities, we have identified opportunities for NIHR to strengthen inclusion and diversity across the research cycle.
NIHR can support more inclusive public partnerships through:
A. Increased funding
Ring-fence a proportion of research funding to support more inclusive engagement. Provide grants (pre and post award) for researchers to establish and sustain community relations, including in dissemination. Implement the learning from existing initiatives. This would help collaborative teams to deepen their expertise and relationships; and allow NIHR to learn how to effectively provide such funding.
B. More joined-up infrastructure
Inclusion cannot be achieved on a project by project basis. Individual research projects are at risk of reinventing the wheel; they cannot provide the foundation for long-term relationships. There is a need to develop and support regional hubs to coordinate activities across the NIHR and with other partners (e.g. NHS organisations and local authorities). Hubs could build relationships of trust with different communities, as the basis for their engagement with research. Hubs could build on the best of what different parts of NIHR already do, and join it up. They could strengthen relationships with community organisations and groups. They could support new roles for brokers/mediators and champions and have the resources to pay for engagement and support.
C. Support, guidance and training
- Establish a strengthened “good practice” repository on Learning for Involvement signalled via NIHR guidance.
- Establish a more formal mechanism to share best practice across research funders.
- Offer coordinated cross-NIHR training on how to promote inclusion in public partnerships. for researchers, NIHR programme staff, public contributors, and public partnerships staff.
D. Strengthening the role of public contributors, and the focus on public partnerships, in funding panels/committees
- Effective scrutiny of public partnership plans. Encourage committees to assess public partnership plans more robustly, e.g. by checking them with studies’ public contributors.
- Develop and support public contributors on committees.
- Encourage innovation. Committees need support to develop and improve. They need time to create a shared vision for public partnerships and to experiment with innovative forms of involvement and engagement.
E. Priority setting that reflects the needs of communities
All funding calls, including proposals for researcher-led calls, should demonstrate that they have taken account of the priorities and experiences of those facing inequalities. This could include linking funding calls to the NHS’s Core20Plus5 programme which identifies specific populations with the worst health access, experience, and/or outcomes.
F. Using NIHR’s influence to promote more inclusive public partnerships
Many EDI issues are systemic. NIHR therefore needs to work with applicants’ host organisations and sponsors and funders of research on the wider challenges. Stakeholder feedback during this Review gave a clear message that change is needed not only within the NIHR but in academia more widely. The NIHR could encourage this by:
- advocating for training on equality, diversity and inclusion for ethics committees
- advocating for reward for inclusive public partnerships in the REF
- establishing a formal mechanism for sharing best practice by research funders
- clarifying its expectations of applicants, sponsors and other funders in regard to EDI.
G. Prioritising inclusion in research on research
Inclusion should be a core priority within the research on research agenda. This means:
- periodic audit of funded research participation and involvement plans, to assess outcomes.
- assessment of the impact of public contributors on funding committees through ethnographic/qualitative research.
- research that informs good practice in partnerships between researchers and marginalised communities
- all research on research, including its priority-setting, should be supported by inclusive public partnerships.
H. Improved dissemination to trial participants and underserved communities
A deeper understanding of health literacy is needed, and of how to disseminate research findings to underserved communities. Those who have taken part in research should be systematically informed of trial outcomes. This could be mandated as part of trial funding.
I. Improved monitoring
To drive improvement, we need a better understanding of the level of diversity in public partnerships across the whole research cycle, from priority setting through to dissemination. There should be routine monitoring of diversity in public partnerships across all NIHR programmes. Building on the wider EDI strategy, guidance is needed on data definitions and governance.
J. Revisiting the supporting questions for the UK Standard for Public Involvement in Research
During our Review, stakeholders asked whether the wording of questions in the UK Public Involvement Standard for Inclusion should be revisited. They are currently framed as “offering opportunities” rather than as a genuine partnership. We would like the Five Nations Public Partnership Group to consider this feedback.
K. A more diverse research workforce
Creating a more diverse research workforce is a core priority in the forthcoming NIHR EDI strategy. The success of this agenda will be critical to supporting more inclusive public partnerships.
L. Alignment with relevant NIHR strategic activity
NIHR is supporting significant activity related to this agenda, including the Under-served Communities programme,the EDI programme and strategy, REPAG and the Race Equality Framework, plus the programme of improvement which is being overseen by the Public Partnerships Programme Board. Coordination across the NIHR to bring these strands of work together, will ensure that the whole is greater than the sum of the parts.
Over the next few months, these recommendations will be worked up into more specific actions that align with, and support, the wider EDI agenda within NIHR. This includes the EDI strategy, due to be published Autumn 2022. We will be seeking endorsement from NIHR leadership, so these recommendations can be taken forward in the work of the NIHR coordinating centres. This is an agenda, not just for the public partnerships community, but for the NIHR as a whole.
Introduction
This Review sets out an Agenda for Action within the NIHR and the research it funds and supports. The Agenda aims to promote health equity and reduce health inequalities through greater inclusion in public partnerships.
The term public partnerships describes ways in which patients, service users, carers and members of the public work with researchers, and health and care professionals, in the creation and use of health and care research. This includes all activities in involvement, participation and engagement.
Figure 1:

Full description of Figure 1:
Public Partnerships is made up of three areas: involvement, engagement and participation. These areas are all connected. Each of these terms is in a circle, and they are arranged in a triangle. Arrows go between each circle. Involvement encourages engagement, and engagement encourages involvement. Participation encourages engagement, and engagement encourages participation. Involvement encourages participation, and participation encourages involvement.
A steering group (membership listed in Annex B), with relevant academic and lived experience expertise, guided the Review. The steering group included 6 public contributors, one of whom was a member of the project team. Public contributors provided additional advice outside of the steering group meetings. A dedicated researcher with expertise in this area, Dr Shoba Dawson, worked collaboratively with a public contributor, Angela Ruddock, to support the Review. We also engaged, through events and interviews, with a range of stakeholders working in public partnerships at national, regional and local level.
The steering group was clear that the final output should be ambitious, and set out an Agenda for Action that would lead to change. The Review explores the wider barriers and enablers to inclusive research. But its recommendations are the actions that the NIHR needs to take.
This Review is not a systematic or comprehensive review of all relevant evidence and guidance. Rather, it is a narrative review based on a range of evidence, including published studies, stakeholder feedback and grey literature. Our steering group had relevant academic and lived experience expertise. This group guided the Review and helped generate actionable insights.
How this report is structured:
- Why promote inclusion in public partnerships?
- The underlying challenges
- The NIHR and the wider context
- How the NIHR is addressing the underlying challenges and the opportunities for improvement
- Recommendations for action and next steps
Why promote inclusion in public partnerships?
“Health and social care research also has a fundamental role to play in helping to reduce the disparities that exist in health outcomes caused by socio-economic factors, geography, age and ethnicity. Working with partners, NIHR needs to tackle the ingrained injustices that exist in the world of research in terms of who is involved, engaged or participating…”
Professor Chris Whitty, Dr Louise Wood,
Best Research for Best Health: The Next Chapter (2021) – NIHR’s current operational priorities.
“We get better science if we are more inclusive”
Professor Lucy Chappell #nihramc21
In the research it funds, the NIHR aims for equality in involvement, engagement and participation. However, respondents to the most recent NIHR Public Involvement Feedback Survey (2020-2021) were predominantly female (57%), 61 years of age and over, White and heterosexual. These public and patient contributors to the NIHR’s work and research highlighted barriers to effective engagement. A key recommendation was to “Support and engage more diverse people to be involved in the NIHR’s work and research to ensure we involve people with a range of knowledge, skills, and experiences”.
A recent study (Bower et al, 2020) found that geographical areas where a disease has most impact, have the lowest numbers of people taking part in related research. This means that diseases which are more common in deprived communities are being studied in healthier populations. The mismatch between the profile of research participants, and the populations who should benefit from the research,means that:
- benefits and side effects of treatments may not translate to real-world patients
- interventions may not be deliverable or applicable to all groups of patients
- findings specific to different populations may be overlooked
- some groups are discriminated against
- changes to health and social care services, based on research recommendations, may not be appropriate for, or acceptable to, everyone.
The recent rapid evidence review of ethnic inequalities in healthcare by the NHS Race and Health Observatory found similarities in experiences of health and care across people from ethnic minority backgrounds. There was a lack of high quality ethnic minority data for research purposes (Kapadia et al, 2022). This, and the lack of inclusion in many studies, means that artificial intelligence could worsen these inequalities (Leslie et al, 2021).
Different ethnic minority groups have different access to, experiences of, and outcomes from health and care services. These differences need to be understood for inequalities to be tackled. In 2015, the NIHR set out its ambition for public partnerships in Going the Extra Mile. This report stressed that unless inclusion in public partnerships is addressed, inequalities in health could get worse.
Public involvement must be diverse and inclusive to enable research that has the potential to reach those that stand to benefit from it most, and thus address issues of health equity
(Islam et al, 2021).
If public partnerships are not inclusive, or if people do not have a genuine opportunity to influence decisions, it undermines the benefits of partnership.
“Our findings suggest that we need more research that acknowledges, investigates and reports on the negative impacts of attempts at public involvement in health research and metrics that measure such involvement. We must ask questions about ways in which public involvement could increase inequalities, distort and suppress rather than amplify particular voices and agendas”
(Russell, Fudge and Greenhalgh, 2020)
Figure 2 maps out the opportunities for public partnerships at all stages of the research (adapted from p14 RDS PPI Handbook). Against this we have identified some of the key benefits (+) and risks (-) from public partnerships (using Brett et al, 2012). If the public partnership is not inclusive it undermines the benefits and magnifies the risks.
Figure 2:
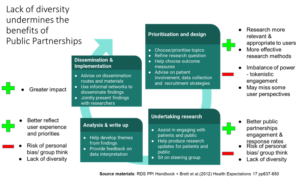
Full description of Figure 2:
The research cycle is made up of different stages including: prioritisation and design; undertaking research;, analysis and write up, and dissemination and implementation. Each of these terms is in a box connected by an arrow to indicate a circular process. For each stage, the opportunities for public partnerships have been indicated in the box. The benefits and risks have also been identified and are indicated next to the relevant box with a plus sign and a minus sign respectively.
For prioritisation and design, public partnerships can help to: choose/prioritise research topics, refine research questions; choose outcome measures and provide advice on patient involvement, data collection and recruitment strategies. The benefits from public partnerships at this stage include research that is more relevant and appropriate to users and more effective research methods. The risks from public partnerships are an imbalance of power and tokenistic engagement and missing some user perspectives.
For undertaking research, public partnerships can help to: engage with patients and public, produce research updates for patients and public, and feed into the steering group. The benefits from public partnerships are better engagement and response rates. The risks are personal bias, group think and lack of diversity.
For analysis and write up, public partnerships can help to: help develop themes from findings and provide feedback on data interpretation. The benefits from public partnerships are better reflections on user experience and priorities. The risks from public partnerships are risk of personal bias, group think and lack of diversity.
For dissemination and implementation, public partnerships can help to advise on dissemination routes and materials, use informal networks to disseminate findings and jointly present findings with researchers. The benefits from public partnerships are greater impact.
The take home message from the diagram is that lack of diversity undermines the benefits of public partnerships. The source materials are the RDS PPI handbook and Brett et al (2012) Health Expectations 17 pp637-650.
Underlying challenges to be addressed
The organisation, Shaping Our Lives, produced the report, Beyond the Usual Suspects, which gives practical guidance on developing more inclusive public partnerships (Beresford, 2013). It describes aspects of who we are, which may not be obvious to others, but which can drive exclusion. Stigma can magnify the problem.
Examples include:
- equality issues – gender, ethnicity, culture, belief, sexuality, age, disability and class
- where we live – homelessness, living in residential services, in prison or secure services, travellers and gypsies
- communication issues – people who are deaf, blind or visually impaired, deaf and blind, those who do not communicate verbally, and people for whom English is not their first language
- impairments – dementia, neurodiversity, people with complex and multiple impairments
- unwanted voices – activists, for example, might be experienced and confident in challenging the status quo.
Inclusive partnerships need to recognise the constellation of factors that give each of us our unique perspective (see figure 3). This is ‘intersectionality’; we each have our own experience of discrimination and privilege. These unique perspectives should be seen as assets, and opportunities to strengthen health and care research.
Figure 3:
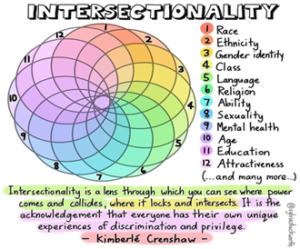
Full description of Figure 3:
Diagram heading reads intersectionality. “Intersectionality is a lens through which you can see where power comes and collides, where it locks and intersects. It is the acknowledgement that everyone has their own unique experiences of discrimination and privilege” – quote from Kimberlé Crenshaw. The diagram shows a rainbow of coloured circles, all slightly overlapping to form a larger circle. The circles are numbered from one to twelve and each circle represents a different characteristic. The characteristics listed are: race, ethnicity, gender identity, class, language, religion, ability, sexuality, mental health, age, education, attractiveness. There are many other characteristics that could be included.
Many scientific papers describe the challenges in developing inclusive public partnerships in research with excluded groups (see bibliography – Annex D). From this evidence, we pulled out two sets of challenges. The first are faced by patients, service users and members of the public. The second are faced by research teams and the organisations they work within. Successful partnerships will be aware of and will address these challenges.
Challenges faced by patients, service users, and members of the public
Public partnerships are more likely to succeed where researchers are aware that patients, service users and members of the public may:
- have had poor and traumatic experiences of research and statutory services
- have experienced stigma and been marginalised
- find it hard to trust you and to see why research would benefit us or those we care for.
- feel intimidated by you
- be embarrassed about our condition or personal circumstances
- find it difficult to express our views in front of people we don’t know
- not have access to digital tools or be able to use them easily
- not have English as our first language
- not be able to read or write easily
- not be able to hear or see easily
- find getting around difficult; we may not have a car or be able to use public transport
- have pressure on our time; we may be in full time work and unable to engage in normal working hours or we may have full time caring responsibilities
- not be clear about our role.
Challenges faced by research teams and the organisations they work in
Public partnerships are more likely to be inclusive and to succeed where researchers and their organisations:
- reinforce the value of public partnerships at all levels and recognise that culture and hierarchies need to change
- reflect the diversity of the communities they work with
- ensure inclusion is a priority for every individual in the wider team, including researchers, public involvement specialists and coordinators, methodologists, reception staff within research clinics
- have the skills and expertise to develop an inclusive partnership process and study design
- are sensitive to cultural context and reflect this in their communication, their engagement, and in the study design
- genuinely share power through authentic, equal and transparent partnerships in which everyone feels valued
- have the financial resources to support inclusive partnerships, and, for example, pay for people’s time, IT, transport or caring costs
- have sufficient time to develop meaningful public partnerships for individual studies and over the longer term
- carry out research on an issue of importance to a group or community, who can see how the research will make their lives better
- offer wider benefits to the community, by mentoring community members who, for example, could achieve an educational qualification as part of the research
- choose people who are known and trusted by the community to carry out the research.
As Ria Sunga of Egality said at a recent NIHR engagement event (Partnering with community organisations to increase diverse voices in research):
“There is no one way to address under-representation in research, it is a very complex issue, and one with many layers.”
To change the culture and ways of working, four related issues need to be addressed:
- Resources – the time and money to overcome barriers to engagement and support inclusive partnerships.
- Partnership skills – to help research teams, university staff, health professionals and engagement leads engender trust and develop reciprocal relationships with communities, respecting and valuing different knowledge bases.
- Wider incentives – to foster a diverse research workforce and inclusive approaches to research. Funders’ expectations of research teams, for example, and criteria for academic success and progression, need to reflect the importance of inclusive partnerships.
- Personal motivation – reinforced by all the above, to engage, share power and create a meaningful partnership.
“Very different ways of working in research are required – where you might start with a community. Research can be good at excluding people – to include them we really need new ways of thinking and working – real culture change. Signals from NIHR about culture and research ways of working have to be powerful and based on a clear set of values and embedded in methods.”
Professor Sophie Staniszewska, Warwick University, Personal Communication
NIHR & wider context
The NIHR report, Going the Extra Mile, Page 19, stated that:
“A diverse and inclusive public involvement community is essential if research is relevant to population needs and provides better health outcomes for all. We have been struck by the degree to which researchers and public contributors have encountered barriers when trying to work with different communities and populations”
Six years later, the engagement work undertaken to support the current NIHR improvement plan for public partnerships (NIHR: Next steps for partnership working with patients and the public, Kaleidoscope Health and Care) identified similar issues. That is, a recognition of the importance of inclusion but frustration at the lack of progress.
The lack of progress cannot be separated from the wider context in which health and care research occurs.
Initiatives such as the Athena SWAN charter demonstrate that interventions can improve gender equity and have a positive impact on equality, diversity and inclusion in academic settings. However, an evaluation of Athena SWAN found challenges to ongoing engagement with Athena Swan include a lack of resources, a lack of support from leadership, and the workload needed to ‘deliver a compelling application’ p55.
Marmot et al (2020) found that austerity had an increasing impact on the quality of life for individuals and communities in England from 2010 to 2020:
“From rising child poverty and the closure of children’s centres, to declines in education funding, an increase in precarious work and zero hours contracts, to a housing affordability crisis and a rise in homelessness, to people with insufficient money to lead a healthy life and resorting to food banks in large numbers, to ignored communities with poor conditions and little reason for hope. And these outcomes, on the whole, are even worse for minority ethnic population groups and Disabled people.”
Marmot et al, 2020
This analysis was conducted before the COVID-19 pandemic, which further exacerbated inequalities. The pandemic impacted the lives of ethnic minority communities, Disabled people or people with impairments, and those living with economic challenge. It also hit the organisations and charities that work with these groups. In this context, inclusion becomes even more important and yet the challenges are increasing.
The NIHR worked with the Health Research Authority, members of the public, patients, service users, other funders, regulators and research organisations to co-produce a Shared commitment to public involvement in research. This commitment builds on the learning from initiatives to strengthen public involvement in research during the COVID-19 pandemic. It ensures people’s perspectives and lived experiences shape the research being planned and delivered.
The shared commitment reiterates the NIHR’s previous assertion to improve inclusion in all that it does. Inclusion was featured as one of the organisation’s 5 operating principles in Best Research for Best Health: The Next Chapter (2021), along with impact, excellence, collaboration and effectiveness. The principle reads:
Inclusion. We are committed to equality, diversity and inclusion in everything we do. Diverse people and communities shape our research, and we strive to make opportunities to participate in research an integral part of everyone’s experience of health and social care services. We develop researchers from multiple disciplines, specialisms, geographies and backgrounds, and work to address barriers to career progression arising from characteristics such as sex, race or disability.
Elsewhere in the document is the pledge:
Expect all research funded and supported by NIHR to demonstrate meaningful, diverse and inclusive involvement, and to show the difference it makes, in line with the UK Standards for Public Involvement and using tools such as the Race Equality Framework.
The NIHR’s approach to public involvement is guided by the UK Standards for Public Involvement in Research (2019). Standard 1 on Inclusive opportunities states:
Offer public involvement opportunities that are accessible and that reach people and groups according to research needs. Research to be informed by a diversity of public experience and insight, so that it leads to treatments and services which reflect these needs.
Standard 1 states that for projects to be inclusive, they need to consider:
- Are people affected by and interested in the research involved from the earliest stages?
- Have barriers been identified and addressed through, for example, payment for time or accessible locations for meetings?
- How is information about opportunities shared, and does it appeal to different communities?
- Are there fair and transparent processes for involving the public in research, and do they reflect equality and diversity duties?
- Is there choice and flexibility in the opportunities offered to the public?
Under this standard, our steering group added:
- Can people genuinely impact the research process and design?
- Can opportunities be co-produced with, or led by, people and communities?
Equality, diversity and inclusion, was another major theme of Public Involvement in Social Care Research, a collaboration between the NIHR and SCIE (Social Care Institute for Excellence). Together, they explored how the NIHR could promote better public partnerships in social care research, and said:
“diversity has to be purposefully addressed – it cannot be left to chance”.
Many initiatives within the NIHR promote this agenda (see Annex C), but they currently lack a clear strategic framework and coordination.
“Clearly the commitment from health/social care leaders to increasing diverse and meaningful involvement is genuine, but we need the voices from those with stories and experiences to share with those leaders” Angela Ruddock, public contributor
The NIHR is committed to improving inclusion in all that it does. Most recently, the role of Head of Equality, Diversity and Inclusion was established and the first EDI strategy for NIHR is due to be published in Autumn 2022. It has 5 strategic themes.
EDI Strategy
The 5 themes are to:
- become a more inclusive funder of research
- widen access and participation for greater diversity and inclusion
- improve and invest in the NIHR talent pipeline
- embed evidence-led diversity and inclusion approaches
- collaborate with partners for impact and sustainability.
The output from this Review will inform the wider EDI strategy and we hope that, together, the Review and the wider strategy will provide a strong platform to argue for the support necessary for successful inclusive public partnerships. That means time, resources and funding.
NIHR: Opportunities for improvement
In this section, we explore evidence from the literature alongside the NIHR’s current activities, to illustrate opportunities for improvement. We conclude this section with a gap analysis of the whole funding cycle to identify areas of particular opportunity.
It is striking that it is relatively rare for publications to describe their own approach to public partnerships, including to diversity. The evidence we call on illuminates key issues, but also has its own limitations and does not reliably capture what matters to communities.
Additional time and resources
One of the most consistent messages from the literature is the need for additional time and resources to foster inclusive public partnerships in research. Building relationships of trust with communities is a time-, resource-, and labour-intensive process (Tembo et al, 2021).
“In any relationship, trust is essential. When you’re building a relationship, if there’s no trust there, you won’t have a very good relationship. So the Community is no different than anybody else. You can’t expect trust back from them, especially if they get the feeling that you don’t have their back or their interest at heart.”
Davine Ford, Public Contributor (NIHR event- Partnering with community organisations to increase diverse voices in research)
Demonstrating trustworthiness can be complex. Trust can be gained or challenged by multiple factors. Partners need to be engaged early and consistently (Heckert et al, 2020); funding calls and project timelines need to allow sufficient time to build relationships and engagement (Bryan et al, 2018, Bonevski et al, 2014). There is an inherent tension between the time needed, and the pressure to generate timely results that can inform clinical practice (Heckert et al, 2020). Stakeholders told us that the speed and timing of NIHR processes can prevent meaningful engagement and the building of trust. Methods that are culturally-appropriate, and can improve access, require funding. They might require interpreters, community brokers, IT equipment, training and mentorship, materials in varied formats and languages. In addition, more complex and less obvious needs can remain unseen, making involvement impossible. The true costs of participation are frequently underestimated (Batty, Humphrey, and Meakin 2022).
“One of the key things to support public contributors, or people with different experiences is providing the training. Giving them that support and building confidence can help them get their voices heard. They’ve got their lived experience, but they just need that support in terms of how you as institutions work and your processes.”
Kirit Mistry, South Asian Health Network (NIHR event- Partnering with community organisations to increase diverse voices in research)
Participant expenses are covered, but few NIHR funding calls make specific allowance for inclusive approaches. Our steering group pointed out that we fund university oncosts. Should we not therefore pay for community oncosts in the same way?
“And it is the responsibility of the researchers, because actually, by looking for the funding what you’re saying to them is – I value your lived experience as much as I value my knowledge. That’s where the equity comes.”
Davine Ford, Public Contributor (NIHR event- Partnering with community organisations to increase diverse voices in research)
Long term relationships with communities
Another consistent theme in the literature, reinforced by our steering group and those we engaged with, is the need for investment that isn’t tied into single research projects, but into long-term relationships (Hickey et al, 2022). Staniszewska et al (2022) talked about “glue money” to sustain relationships between researchers and communities outside of formal research projects.
A recent scoping review, conducted for the NIHR, stated:
“The fragmentation of regional NIHR public involvement resource into separate centres, programmes and projects, with finite contracts and funding, also impacts on the ability of public involvement teams to successfully build and maintain trusting relationships with public contributors and communities, and to build capacity. These relationships are crucial in supporting teams to develop and deliver e.g. funding bids within the short timescales demanded by NIHR funding panels. However, they require a significant amount of time and stable resource to establish and maintain. In the current model, individual research teams do not have the resource or capacity to reach out into local communities in anything other than a piecemeal way.”
Increasing Diversity on National Funding Committees: A Scoping Review – Smith, 2021
Islam et al’s (2021) proposed that:,
“Maybe there should be ‘how to involve researchers in communities’ rather than involving communities in research”
Islam et al (2021).
Our steering group strongly support this proposal.
Suggestions to sustain relationships with local communities include:
- Establish and use multiple links to diverse communities. For example, using engagement events, speaking opportunities and personal links with key individuals and organisations (Waheed et al, 2015, den Oudendammer et al, 2019)
- Build a list of brokers and mediators with strong links to diverse communities and fund them to engage and facilitate dialogue between funders, universities and these communities. (Bryan et al, 2018, Waheed et al, 2015, Bodicoat et al, 2021)
- Create a research participant registry for improved access to participants from disadvantaged communities (Bonevski at al, 2014).
- Provide spaces for engagement activities that are safe and welcoming (Bryan et al, 2018).
At several of our engagement events, people argued that a regional hub with permanent staff could help establish and maintain long-term relationships. A hub could pool funding, expertise and resources across different projects. It could support community networks in a region and avoid duplication.
Inclusion within research proposals
Funding panels and committees
Funding panels need to reflect the diversity of the UK population (Bryan et al, 2018, den Oudendammer et al, 2019). The NIHR should publish data on the ethnic make-up of decision-making bodies and on application-award success (Bryan et al, 2018). A recent scoping review for the NIHR (Smith, 2021) highlighted the lack of diversity on panels and variation in how they operate. Smith stated that panels of academics and clinicians can be a hostile environment for inexperienced public contributors, who can feel their contribution is tokenistic. Having a public contributor co-Chair was proposed as a way of raising the profile of the public voice within panels. The co-Chair might need support and training. Another proposed solution was restructuring the review process such that the public contributor speaks first instead of third.
“That system, I think, by its very nature, makes inclusion much more difficult because it makes people feel less welcome… it requires particularly sensitive chairing skills to help people be involved”
Graham, Public Contributor (NIHR event- Partnering with community organisations to increase diverse voices in research)
Staniszewska et al (2021) looked at public partnerships on funding committees/panels and made 16 high level recommendations, including:
- extending the diversity of committee membership
- greater feedback on public contributor experience
- developing a whole committee vision of public partnerships
- strengthening the voice of the public contributor in the committee’s operation.
Expectations of proposals
Engagement can start even before funding has been secured. In this way, partners can influence research questions and design, and encourage team building (Snape et al, 2014). Small grants from the NIHR Research Design Service have been helpful in promoting engagement in the development of applications (Boote et al, 2015). The NIHR should challenge proposals that fail to demonstrate a clear understanding of ethical partnerships (Bryan et al, 2018) or whose study design is not appropriate for the cultural context (George, Duran, and Norris 2014). Reviewers require training to assess inclusiveness and prioritise trials that sample underrepresented groups (Smart, 2021). Funders should provide examples of what a “good” proposal would look like (Bryan et al, 2018)
Upskill the research workforce
Working collaboratively with communities with diverse cultures and experiences requires training.
“Do we know how to engage? I know it sounds like a silly question. But in order to bring people along with us; do we know where to find them; do we include them in our planning stages; do you know what methods to use to involve them; do we know how people want to be involved? These are a few of the questions that come up time and time again.”
Davine Ford, Public Contributor (NIHR Event – Partnering with community organisations to increase diverse voices in research)
The community engagement conducted to support NIHR’s race equality framework demonstrated the importance of acknowledging that many communities have a history of “harm, betrayal, trauma” caused by racial injustices. As other research has highlighted (Ocloo et al, 21), there is wide mistrust of research and researchers. Addressing issues of mistrust, and the underlying imbalance of power, is critical to successful engagement (Banas et al, 2019, Bryan et al, 2018, Beresford, 2013). Waheed et al (2015) and others have encouraged cultural competency training for researchers and placements to help them appreciate community needs. However, some have challenged the concept of cultural competence, particularly in medical settings, as potentially simplifying cultures and overlooking the differences between people (Kleinman and Benson, 2006).
“Cultural humility” therefore becomes as important. This means individuals embedding a practice of “self-reflection and self-critique as lifelong learners…”
checking power imbalances that exist because of people’s roles, and
“develop[ing] and maintain[ing] mutually respectful and dynamic partnerships with communities…”
(Tervalon and Murray-García, 1998). Researchers will need to consider how they will build effective partnerships with community-based organisations (Turin et al, 2022) including through training and support.
“It takes time for researchers who are new to the field of co‐research or dementia to see people with dementia as individuals with knowledge and experience rather than members of a category associated only with impairment.”
(Waite, Poland, and Charlesworth 2019)
Researchers need to see the value of partnerships, to both researcher and participant, and to address the imbalance of power inherent in the relationship (Chambers et al, 2019). Participatory design principles and engagement techniques such as drama, video, pictures and objects can help redress the power imbalance (Broomfield et al, 2021, Bryan et al, 2018). Other techniques to strengthen reciprocal relationships and communication exist (Farr et al, 2021).
Inclusive partnerships support the dissemination of research outcomes
The evidence suggests that the dissemination of research frequently lacks inclusive public partnerships, even though partnerships can promote its reach and impact (Dawson et al, 2018).
“Is disseminating results to participants in language and terms they understand prioritised? There is a long way to go, currently only 10% of research gives the results to participants (HRA figures). If we aren’t doing this with existing research participants, how can we possibly hope to achieve it with underserved communities?”
Lynn Laidlaw, Public Contributor, Steering Group Member
Communities want to see the benefit and outcome of their engagement. Effective dissemination of outcomes is one way of doing this. Feedback needs to be relevant, accessible, and free from jargon (Farooqi et al, 2022). Recent research, commissioned by the NIHR from Kingston/St George’s University (Bearne et al, 2022), made a series of recommendations about how to reach more diverse communities. These include:
- more tailored approaches which use language and media (written or digital approaches, for example) familiar to each audience
- using trusted intermediaries to support communication
- including stories of lived experience.
Evaluate the impact of new approaches
Stakeholders we engaged with emphasised the need for experimentation and innovation, but said that new approaches to embed inclusive partnerships need to be evaluated. They felt the NIHR tends not to evaluate its own initiatives.
Resources are needed to evaluate public involvement (Boivin et al, 2018; Snape et al, 2014). Approaches for evaluation should be developed with people with lived experience (Laidlaw, 2021, Boivin et al, 2018), and should acknowledge the complexity, and capture the learning that is integral to this way of working (Boivin et al, 2018; Staley, Abbey-Vital, and Nolan 2017). Overall, there is a need for a more robust evidence base –
“Further progress towards making patient and other stakeholder engagement in research more widely practised can be made if researchers, stakeholders, institutions, funders, and policy makers learn together about the key challenges and act together through further research, capacity building, and policy change.”
(Heckert et al, 2020)
Whole system incentives and support for wider cultural change
Because many EDI issues are systemic, the NIHR needs to work with academia and other funders on the wider challenges. A strong message from our engagement with stakeholders during the Review was that change is needed not only within NIHR but in academia more widely. The NIHR needs to use its influence to encourage this.
“Culture change is at the heart of this. Otherwise we are involving underserved communities in an environment that isn’t fit for purpose. We need to explicitly acknowledge the things that are challenging, including research hierarchies, in order for anything to change.”
Lynn Laidlaw, Public Contributor, Steering Group Member
Incentives to promote inclusion are needed at individual, organisation and system levels (Ayton et al, 2021, Ocloo et al, 2021). They should be embedded and reported across the whole research system including institutions, ethics committees, journals and funders (Snape et al, 2014). Ethnicity data needs to be collected and used diligently (HSRUK et al, 2022).
This requires a culture change across the whole system. Inclusive public partnerships need to move from being a tick-box exercise to a valued agenda that is seen as core to delivering high quality research and impact.
“If this doesn’t happen, then we will get a tick box EDI, eg researchers saying to PPI leads “find me a public contributor with certain characteristics such as ethnic community etc”
Lynn Laidlaw, public contributor, Steering Group Member
Without culture change we risk involving underserved communities in an environment that could cause as much damage as benefit to those who we engage with.
The Runnymede Trust set out 10 principles for community-university partnerships to promote non-exploitative relationships.
The 10 commitments are to:
- strengthen the partnering community organisation
- seek mutual benefit
- transparency and accountability
- fair practices in payments
- fair payments for participants
- fair knowledge exchange
- sustainability and legacy
- equality and diversity
- sectoral as well as organisational development
- reciprocal learning
Standardised methods for recording diversity
Recent work by Egality, working with medical research charities, highlighted that ethnicity data is not routinely collected. This means organisations and the research sector don’t know the diversity of participants currently involved in research, and don’t have a benchmark to measure improvement. The lack of standardised methods and inclusive categories means researchers don’t feel equipped to record ethnicity. Egality recommended that national bodies work together to develop standardised methods and inclusive categories to help researchers to record and report ethnicity.
Reinforcement within academia
The published literature singles out the frequent mismatch between support for co-production, which takes time, and academic incentives, including the Research Excellence Framework (REF), which rewards researchers for the number of publications they produce. Feedback from stakeholders, including our steering group, highlighted the challenges created by short-term contracts for researchers, and the wider pressures that academics are under. Public engagement often struggles to compete for time and resources within the context of a system driven by reward and recognition for research itself (Hamlyn et al, 2015).
“Even good intentions and well-planned engagement activities can be diverted
within the existing research funding and research production systems where non-research stakeholders remain at the margins and can even be seen as a threat to academic identity and autonomy.”
(Boaz et al, 2021)
Academia and research funders need to value interdisciplinary and team science, and the skills that foster co-production (Tembo et al, 2021). As a key stakeholder in REF development, and a significant funder of University activity, the NIHR could promote the value of inclusion.
The Research Excellence Framework could incorporate a mechanism that values and rewards the outputs of co-production (for example the total number of peer-reviewed articles that are single authorship or lead authored with community partners; evaluating how the research contributed to strengthening local community participation, skills building, research literacy, or creative engagement) and measures the effect of research on people’s lives.”
(Tembo et al, 2021)
Diversity within the research workforce
A more diverse research workforce will encourage and support more inclusive public partnerships (Chambers et al, 2017, Prinjha et al, 2020). Action is needed to encourage this.
“This is not said enough times. The makeup of the workforce is so important in improving and ensuring real dialogue and collaboration.”
Angela Ruddock, Public Contributor
Marginalised academics lack visibility, even within research on diversity, equity and inclusion, and are often employed on zero hours contracts (HSRUK et al, 2022). The commitment to end discrimination on the grounds of race, ethnicity, religion, language or cultural tradition needs to be made explicitly. It needs to be part of the grant awarding processes, including peer review. (Bryan et al, 2018)
Action across the whole research cycle
Partners should have the opportunity to be involved at every stage: from setting priorities and questions to data collection, analysis and dissemination (HSRUK et al, 2022). Engagement across the whole research cycle from the initial concept to implementing findings can help engender trust in research (George et al, 2014).
Below we assess the degree to which NIHR promotes inclusion across the research cycle. This highlights the opportunities for improvement at all stages. This assessment informs the final recommendations.
“The widening of involvement needs to occur in all research stages from prioritisation of topics, through conceptualising projects, commissioning processes, conducting studies and reporting and seeking impact from them”
(Clark et al, 2021 p1547)
Assessment of current NIHR support for inclusive engagement
Engagement is essential across the research cycle. Here we look at:
- Deciding on research priorities
- Making funding decisions
- Supporting research design and delivery
- Supporting the dissemination of research findings
- Evaluating the outcomes of research
- Working with other funders to share best practice
- Whole system action – including a more diverse research workforce
Deciding on research priorities
Current support
- James Lind Alliance (JLA) brings patient, carer and clinician groups together on an equal footing to identify research priorities using inclusive communications methods. JLA is a pilot partner for the NIHR’s race equality framework. Its work informs the priorities of the Health Technology Assessment and other NIHR research programmes. Research on the JLA has shown that the priorities of people living with conditions differ distinctly from those delivering care (who often conduct the research); there is also a need to strengthen the influence of those with lived experience on funding and funders (Staley et al, 2020).
- Research for Patient Benefit
Working with Public Contributors to develop a Proposal Development Grant call for proposals that work with PPI in novel and innovative ways within communities and as partnerships. The call will be launched in Summer 2022
The NIHR Public Health Research Programme has launched funding calls which encourage inclusion of geographic populations which have been historically under-served. The calls aim to boost research in the areas with the greatest health needs. Past examples include:
- Increasing uptake of vaccinations in populations where there is low uptake
- Digital health inclusion and inequalities
- What are the health and health inequality impacts of being outdoors for children and young people?
Potential for improvement
- Routine monitoring of inclusion (public partnerships) in priority setting across all NIHR programmes.
- All funding calls, including proposals for researcher-led calls, should demonstrate that they have taken account of the priorities and experiences of those facing inequalities.
- Funding should be available to support community engagement in developing proposals.
Making funding decisions
Current support
- PPI guidance for NIHR applications encourages diversity but there is no data to tell us how systematically it is adhered to.
- NIHR Funding Committees/Panels currently lack diversity, including among their public contributors.
- HSDR is trialling an approach in which equality, diversity and inclusion is assessed when applications are reviewed; ‘inclusion observers’ provide feedback.
- NIHR’s Global Health Research programme expects all research to be undertaken in collaboration with the communities most likely to be affected by the research outcomes. It provides guidance on participatory approaches.
Potential for improvement
- Routine monitoring of inclusion (public partnerships) on panels.
- More robust assessment of public partnership plans potentially checking them with public contributors.
- Regular audit to check outcomes of participation and involvement plans for funded research.
- More systematic feedback on the experience of public contributors on funding panels/committees.
- Explore the impact of public contributors on funding sub-committees through ethnographic and qualitative research.
- Provide support for the development and improvement of committees. They need time to create a shared vision for public partnerships and to experiment with innovative forms of engagement.
Supporting research design and delivery
Current support
- NIHR has provided researchers with support. For examples and prompts for best practice, see Annex C.
- NIHR Digital strategy is developing a research registry to support more diverse engagement.
- The NIHR Patient Engagement in Clinical Development Service is encouraging life science companies to involve patients to “help shape and improve the design and, ultimately, the delivery of commercial clinical research”.
- Services connect specific population groups with research. This includes ensuring children and young people influence new medical devices and medical technologies.
- Many examples of NIHR fora and approaches are connecting people and communities from diverse backgrounds (including young people, homeless populations etc) with researchers.
Examples of additional support for engagement: regular, small amounts of funding from the NIHR Research Design Service for engagement in the development of grant applications; a NIHR pilot funding programme provided up to £10,000 for proposals to strengthen public partnerships in specific regions/geographies; larger funds to ‘Develop innovative, inclusive and diverse public partnerships’.
- Payment for PPI engagement; guidance on how to pay.
Potential for improvement
- Provide separate funding to support more inclusive and community engagement.
- Routine monitoring of the degree to which public partnerships in research were genuinely inclusive
- Lack of long-term relationships but regional infrastructure for PPI is being explored and mapping work undertaken. A proposal for regional hubs is being developed by NIHR for consideration by DHSC.
- Encourage follow on applications that allow collaborative teams to deepen their expertise and relationships.
- NIHR guidance to strengthen a repository of examples of good practice.
Supporting the dissemination of research findings
Current support
- Open Access Policy
- NIHR Evidence – providing accessible summaries of NIHR outputs with public contributors on the editorial board, and as reviewers.
- Learning from research on how to better reach underserved communities.
- Guidance to create inclusive content and language
- Journals Library – Reporting Equality, Diversity and Inclusion in PPI (nihr.ac.uk)
- The National Elf Service disseminates good quality evidence from multiple sources in accessible ways, and the NIHR School of Social Care is one of the organisations behind the Social Care Elf.
- The NIHR-funded Piper Study starting in Autumn 2022 is exploring the role of patients and the public in the implementation of evidence into practice.
- Co-creating communication, engagement and dissemination with minoritised communities and ensuring outputs are accessible.
Potential for improvement
- Require researchers to feedback to communities and research participants on the outcome of the research they have participated in.
- Engage communities around what dissemination approach works best for them and who they feel should be the target audience e.g. are these messages GPs need to hear?
- Act on audience research findings, including insights about health literacy, to better reach underserved communities.
Evaluating the outcomes of research
Current support
- No systematic use of inclusive public partnerships in NIHR’s research on research and evaluation programme.
Potential for improvement
- Inclusion should be a core priority within the research on research agenda.
- Systematic public engagement in setting priorities for and engagement in research on research and evaluation.
Working with other funders to share best practice
Current support
- NIHR works closely with HRA and others – see shared commitment to “meaningful, diverse and inclusive involvement”.
- NIHR Health Technology Assessment programme has been working with PCORI, sharing best practice in engaging patients, stakeholders, and underserved groups in research.
Potential for improvement
- Establish a more formal mechanism to share best practice in this area across research funders.
- Create consistent monitoring variables.
Whole system action – including a more diverse research workforce
Current support
- NIHR feeds into REF reviews.
- NIHR Academy encouragement of diversity in NIHR research professorships
- NIHR forthcoming EDI strategy will address diversity across NIHR
- Vocal in Greater Manchester is an example of shared infrastructure for inclusive public partnerships, resourced by health and care research initiatives across a region and shaped with people and communities from diverse backgrounds or with varied experiences to articulate and respond to local priorities.
Potential for improvement
- Advocate training for ethics committees on equality, diversity and inclusion and partnership working
- Advocate for equality, diversity and inclusion and reward for inclusive public partnerships in the REF.
- Ensure forthcoming NIHR EDI strategy includes action to monitor and address diversity in the research workforce.
Conclusion, recommendations for action & next steps
A long history of exclusion in society has left a legacy of deep-seated health inequalities. Exclusion from society has led to the lack of inclusion in research and practice, which further increases health inequalities. These inequalities then reinforce the disadvantage embedded in wider society and culture. We need to break the cycle of exclusion and inequality.
In order to do this, our steering group and those we engaged with, told us that we need to reframe the relationship between researchers and communities. We need to ensure that people have the platform and power to influence, inform and initiate research.
We should not expect the public to fit into research systems. Instead, we need to help researchers get closer to communities. NIHR needs to create systems to facilitate this. In particular, systems that can help redress the imbalance of power and the mistrust frequently felt by communities towards research and researchers. For communities, research is not an end in itself but should be a route to a better life. This connection is rarely seen. Inclusion is not only about race but all marginalised and excluded communities. The whole system needs a change of culture. Inclusive public partnerships need to move from being a “tick box exercise” to a valued agenda that is core to delivering high quality research and impact. This will take time, resources and effort, along with a significant change in research culture.
While this Review explores the wider barriers and enablers to inclusive research, its recommendations are directed towards the actions that NIHR needs to take. The Review has identified notable examples of good practice within and outside of NIHR (see Appendix C). Many researchers are already working with communities, and building trusting relationships in collaborative partnerships that empower people. We have identified many opportunities for NIHR to strengthen inclusion and diversity across the research cycle.
NIHR can support more inclusive public partnerships through:
A. Increased funding
Ring-fence a proportion of research funding to support more inclusive engagement. Provide grants (pre and post award) for researchers to establish and sustain community relations, including in dissemination. Implement the learning from existing initiatives. This would help collaborative teams to deepen their expertise and relationships; and allow NIHR to learn how to effectively provide such funding.
B. More joined-up infrastructure
Inclusion cannot be achieved on a project by project basis. Individual research projects are at risk of reinventing the wheel; they cannot provide the foundation for long-term relationships. There is a need to develop and support regional hubs to coordinate activities across the NIHR and with other partners (e.g. NHS organisations and local authorities). Hubs could build relationships of trust with different communities, as the basis for their engagement with research. Hubs could build on the best of what different parts of NIHR already do, and join it up. They could strengthen relationships with community organisations and groups. They could support new roles for brokers/mediators and champions and have the resources to pay for engagement and support.
C. Support, guidance and training
- Establish a strengthened “good practice” repository on Learning for Involvement signalled via NIHR guidance.
- Establish a more formal mechanism to share best practice across research funders.
- Offer coordinated cross-NIHR training on how to promote inclusion in public partnerships. for researchers, NIHR programme staff, public contributors, and public partnerships staff.
D. Strengthening the role of public contributors, and the focus on public partnerships in funding panels/committees
- Effective scrutiny of public partnership plans: encourage committees to do more robust assessment of public partnership plans, eg by checking them with studies’ public contributors.
- Develop and support public contributors on
- Encourage innovation. Committees need support in order to develop and improve. They need time to create a shared vision for public partnerships and to experiment with innovative forms of involvement and engagement.
E. Priority setting that reflects the needs of communities
All funding calls, including proposals for researcher-led calls, should demonstrate that they have taken account of the priorities and experiences of those facing inequalities. This could include linking funding calls to the NHS’s Core20Plus5 programme which identifies specific populations with the worst health access, experience, and/or outcomes.
F. Using NIHR’s influence to promote more inclusive public partnerships
Many EDI issues are systemic. NIHR therefore needs to work with applicants’ host organisations and sponsors and funders of research on the wider challenges. Our engagement during this Review gave a clear message that change is needed not only within the NIHR but in academia more widely. The NIHR could encourage this by:
- Advocating for training on equality, diversity and inclusion for ethics committees.
- Advocating for reward for inclusive public partnerships in the REF.
- Establishing a formal mechanism for sharing best practice by research funders.
- Etrengthening what NIHR says regarding its clear expectations of applicants, sponsors and other funders in regard to EDI.
G. Prioritising inclusion in research on research
Inclusion should be a core priority within the research on research agenda. This means:
- Periodic audit of funded research participation and involvement plans, to assess outcomes.
- Assessing the impact of public contributors on funding committees through ethnographic/qualitative research.
- Research that informs good practice in partnerships between researchers and marginalised communities.
- All research on research, including setting research on research priorities, should be supported by inclusive public partnerships.
H. Improved dissemination to trial participants and underserved communities
A deeper understanding of health literacy is needed and how to disseminate research findings to underserved communities. Those who have taken part in research should be systematically informed of trial outcomes. This could be mandated as part of trial funding.
I. Improved monitoring
To drive improvement, we need a better understanding of the level of diversity in public partnerships across the whole research cycle from priority setting through to dissemination. There should be routine monitoring of diversity in public partnerships across all NIHR programmes. Building on work in the wider EDI strategy – guidance is needed on data definitions and governance.
J. Revisiting the supporting questions for the UK Standard for Public Involvement in Research
During our Review, stakeholders asked whether the wording for the current questions for the UK Public Involvement Standard for Inclusion should be revisited. They are currently framed as “offering opportunities” rather than as a genuine partnership. We would like the Five Nations Public Partnership Group to consider this feedback.
K. A more diverse research workforce
Creating a more diverse research workforce is a core priority in the forthcoming NIHR EDI strategy. The success of this agenda will be critical to supporting more inclusive public partnerships.
L. Alignment with relevant NIHR strategic activity
NIHR is supporting significant activity related to this agenda, including the Under-served Communities programme,the EDI programme and strategy, REPAG and the Race Equality Framework, plus the programme of improvement which is being overseen by the Public Partnerships Programme Board. Coordination across NIHR to bring these strands of work together will ensure that the whole is greater than the sum of the parts.
Next steps
Over the next few months, these recommendations will be worked up into more specific actions that align with and support the wider EDI agenda within NIHR, including the EDI strategy to be published in Autumn 2022. We will be seeking endorsement from NIHR leadership, so they can be taken forward in the work of the NIHR coordinating centres. This is an Agenda, not just for the public partnerships community, but for the NIHR as a whole.
Paper authors and how to cite this report
Candace Imison, Meerat Kaur, Shoba Dawson
Imison C, Kaur M, Dawson S. Supporting equity and tackling inequality: how can NIHR promote inclusion in public partnerships?, An agenda for action; August 2022, [URL], (Accessed on: [DATE])
Annex A – Glossaries
Glossary – Equality, Diversity and Inclusion
Access and Outreach – the activity undertaken to support underrepresented groups to access higher education. This may include:
- Sustained and progressive programmes of targeted outreach with schools, colleges and job centres.
- Broader collaborative activities with employers, third sector organisations and other education providers.
Advocate – someone who speaks up for themselves and others, e.g. a person who lobbies for equal pay for a specific group.
Carer and Caring responsibility – a carer is a person who has total or substantial responsibility for helping and supporting another person. This could be a partner, a parent, a child, other relative, friend or neighbour. This might be necessary because of age, physical or mental illness, learning difference, addiction, disability, or other factors. A carer can be an adult, child or young person.
Cognitive diversity – the different perspectives, ways of thinking and different skill sets that people from different backgrounds and diverse experiences have. In an EDI context, it is often used to emphasise the benefits of including different people in order to provide a variety of perspectives, ways of thinking and ideas.
Dignity – a value owed to all humans, to be treated with respect.
Diversity – everyone is different in a variety of visible and non-visible ways, and that those differences are to be recognised, respected and valued.
Equal opportunities – or equality of opportunity, ensures that everyone is entitled to freedom from discrimination, and has an equal opportunity to access opportunities and fulfil their potential. The term ‘equal opportunities’ has mostly been replaced by ‘equality, diversity and inclusion’ in recent years.
Equality – is about ensuring that every individual has an equal opportunity to make the most of their lives and talents. Noone should have poorer life chances because of where, what or whom they were born, or because of other characteristics. Equality recognises that certain groups of people with particular characteristics e.g. those of a certain race, with disabilities, women, gay and lesbian people etc, continue to experience discrimination.
Equality Impact Assessment – is abbreviated to EIA or sometimes EQIA. A detailed and systematic analysis determines how a policy, procedure or change to process may disproportionately impact a particular group.
Equity – the proposition that individuals should be provided with the resources they need to have access to the same opportunities as the general population. Equality indicates uniformity and the even distribution of resources among all people. However, equity represents the distribution of resources in such a way as to meet the specific needs of individuals. It acknowledges that some groups and individuals require more or less resources in order to access the same opportunities as others. Treating everyone equally does not necessarily lead to equality; equal treatment often perpetuates existing hierarchies.
Human rights – the basic rights and freedoms to which all humans are entitled. They ensure people can live freely and are able to flourish, reach their potential and participate in society. These rights help to ensure that people are treated fairly and with dignity and respect. An individual has human rights by virtue of being human and they cannot be taken away.
Identity – the characteristics and qualities of a person, considered collectively, which are essential to that person’s self-awareness. A dimension of an individual’s identity is their relation to a collective group identity, which is often socially constructed. This means that a generalised view of an individual’s identity, based on their perceived association with a group, may be formed and may lead to harmful stereotypes, disadvantages and discrimination.
Inclusion – the creation of a learning, working and social environment that is welcoming, which recognises and celebrates difference and is reflected in structures, practices and attitudes.
Inclusive language – refers to non-sexist language or language that “includes” all persons in its references. For example, the statement “a writer needs to proofread his work” excludes women due to the masculine reference of the pronoun. Likewise, “a nurse must disinfect her hands” excludes men and perpetuates the stereotype that all nurses are women. Therefore, unless a sentence refers to a specific person, it is better to use language that is inclusive of all. This is especially important in policies and procedures. Also see the ‘Gender neutral’ definition.
Intersectionality – the idea that an individual’s identity consists of various biological, social and cultural factors, including race, ethnicity, gender, religion and sexual orientation etc, and that each of these contributes to their overall identity and to who they are as an individual. The theory of intersectionality was originally coined by Kimberlé Crenshaw, an American civil rights activist, to describe the specific inequalities faced by African-American women. The term is now used more broadly, and a single person may experience multiple forms of discrimination and systematic social inequality as a result of belonging to more than one social category simultaneously. It may also mean that they experience privileges or disadvantages because of different aspects of their identity. They may experience barriers or even be excluded from one particular group as an indirect result of their identification with another. Also see the ‘Lived experience’ definition.
Lived experience – the unique knowledge an individual gains through direct, first-hand experience of living their life, while identifying with one or more protected characteristic, such as race, religion or sexual orientation etc. Lived experience refers to a person’s understanding of what life is like for them as a unique individual, how they are treated by others, and their experience of navigating the systems and processes embedded in society.
In an EDI context, lived experience also refers to different forms of direct and/or indirect discrimination that an individual may face due to their actual or perceived association with a particular group or protected characteristic. The discrimination that individuals face is unique to them and may be impacted by the intersection of other aspects of their identity as they identify with multiple protected characteristics. Also see the ‘Intersectionality’ definition.
Protected characteristic – a term used in the Equality Act 2010 to describe people’s characteristics, in relation to which they are protected against discrimination
and harassment. Under the Act, there are 9 protected characteristics: age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion or belief, sex, sexual orientation. More information about these terms can be found in the Equality and Human Rights Commission glossary of terms.
Public Sector Equality Duty (PSED) – means that public bodies have to consider all individuals when carrying out their day-to-day work: in shaping policy, in delivering services and in relation to their own employees. TPSED came into force across Great Britain on 5 April 2011.
It also requires that public bodies have due regard to the need to:
- eliminate discrimination
- advance equality of opportunity
- foster good relations between different people when carrying out their activities
Respect – taking into account the views and desires of others.(This definition has been taken from the Equality and Human Rights Commission glossary of terms.)
Tokenism – the practice of making only superficial or symbolic gestures to appear inclusive of members of underrepresented or minoritised groups. For instance, by recruiting people from minority ethnic groups, an organisation may give the appearance of racial integration or balance within a workforce, but may make no further efforts to invest additional resources into exploring the root cause of such imbalance, or to improving the experiences of minority groups once they are part of the workforce. Also see the ‘Performative’ definition.
Unconscious Bias – the unconscious associations and beliefs that form outside of our own conscious awareness, which lead to positive or negative inclinations towards or against other people, groups or communities.
Unconscious biases can lead to stereotyping and interfere with impartial judgement and decision-making. They have been shown to influence recruitment and selection decisions, as people tend to form positive associations for those who are like them, which leads to more negative outcomes for those people who are not like them.
Although the effectiveness of unconscious bias training has been debated, its purpose is to help people recognise when they are making a decision based on an unconscious belief or assumption. It aims to help people develop practical tools to mitigate the negative impact that a bias may have upon decision-making in the moment.
Underrepresented groups – groups of people who are insufficiently or inadequately represented, relative to their representation in broader society. People within these groups may be subject to barriers and forms of discrimination.
Glossary – NIHR
A full glossary is available on the NIHR glossary page.
Clinical trial
An experiment to compare the effects of two or more healthcare interventions. ‘Clinical trial’ is an umbrella term for a variety of healthcare trial designs.
Collaboration
Active, on-going partnership with members of the public in the research process. For example, members of the public might take part in an advisory group for a research project, or collaborate with researchers to design, undertake and/or disseminate the results of a research project.
Commissioned calls
Calls for proposals based on pre-defined research questions developed to respond to the information needs of decision-makers (typically, but not exclusively, within the NHS).
Co-production
An approach in which researchers, practitioners and the public work together, sharing power and responsibility from the start to the end of the project, including the generation of knowledge. The assumption is that those affected by research are best placed to design and deliver it and have skills and knowledge of equal importance.
Dissemination
Communicating the findings of a research project to a wide range of people who might find it useful. This can be done through producing reports, publishing articles in journals or newsletters, issuing press releases or giving talks at conferences.
Empowerment
The process by which people who use services equip themselves with the knowledge, skills and resources they need to take control over decisions and resources. It often involves them building confidence in their own strengths and abilities. It does not always mean people taking control over all decisions or all resources.
Engagement
Ways in which research can be shared with the public in a 2-way process. Engagement encourages researchers to listen and interact with the general public, for example, via science festivals, open days, media coverage.
Ethics committees
Committees that make sure research respects the dignity, rights, safety and well-being of the people who take part. Increasingly, ethics committee approval is needed for health and social care research. Ethics committee members include researchers and health care professionals as well as members of the public.
Evaluation
An assessment of whether an intervention (for example, a treatment, service, project, or programme) is achieving its aims. A project can be evaluated as it goes along or right at the end. An evaluation can measure how well the project is being carried out as well as its impact. The results of evaluations can help with decision-making and planning.
Evidence base
A collection of all the research currently available on a health or social care topic, such as how well a treatment or a service works. This evidence is used by health and social care professionals to make decisions about the services they provide, and what care or treatment to offer.
Evidence synthesis
The development of techniques to combine multiple sources of quantitative and qualitative data to derive best evidence for use in healthcare.
Experts by experience
This term refers to service users and carers, who are experts through their experience of illness or disability and services.
Funding committee or panel
A group of experts who consider grant applications and reviewer reports to decide whether to recommend funding.
Health Research Authority (HRA)
The Health Research Authority (HRA) is an NHS organisation established to protect and promote the interests of patients and the public in health research.
Health Protection Research Units (HPRUs)
Health Protection Research Units (HPRUs) are 13 research partnerships between universities and Public Health England (PHE); they act as centres of excellence in multidisciplinary health protection research in England.
Health Technology Assessment (HTA)
The HTA Programme produces independent research information about the effectiveness, costs and broader impact of healthcare treatments and tests for those who plan, provide or receive care in the NHS.
James Lind Alliance (JLA)
An initiative that brings patients, carers and clinicians together in Priority Setting Partnerships (PSPs). Together, they identify and prioritise the top 10 unanswered questions or evidence uncertainties in a specific condition, area or topic.
Journal
A publication in which researchers formally report the results of their research to people who share a similar interest or experience. Journals often specialise in one topic.
Lay (lay person)
The term means non-professional. In research, it refers to the people who are neither academic researchers nor health or social care professionals.
Methodology
The term describes how research is done. It covers how information is collected and analysed, as well as why a particular method has been chosen.
NHS
National Health Service: Government-funded medical and health care services that everyone living in the UK can use without being asked to pay the full cost of the service.
NIHR Academy
The NIHR Academy is responsible for development and coordination of NIHR academic training, career development and research capacity development.
NIHR Applied Research Collaborations (ARCs)
NIHR ARCs support applied health and care research that responds to, and meets, the needs of local populations and local health and care systems. These 15 local partnerships between NHS providers, universities, charities, local authorities, Academic Health Science Networks and other organisations also undertake implementation research to increase the rate at which research findings are implemented into practice.
NIHR Biomedical Research Centres (BRCs)
NIHR’s 20 BRCs are collaborations between world-leading universities and NHS organisations that bring together academics and clinicians to translate lab-based scientific breakthroughs into potential new treatments, diagnostics and medical technologies.
NIHR Centre for Engagement and Dissemination (CED)
The NIHR CED focuses on two aspects of the NIHR mission. First, we champion the effective engagement and involvement of patients, public, carers, service users and communities (people and communities) in all parts of the research journey. Second, through our support for dissemination and mobilisation of evidence, we stimulate the translation of research findings into policy and practice to improve patient outcomes and health and social care services.
NIHR Clinical Research Network (CRN)
NIHR CRN funds and coordinates some 14,000 research support staff in every single NHS Trust in England, in thousands of GP practices, and in numerous other research sites including care homes, hospices, local authorities, dental surgeries, schools, and prisons.
Participant
An individual who is studied in a trial, often, but not necessarily, a patient.
Participation
The act of taking part in a research study, for example people being recruited to take part in a clinical trial or another kind of research study, joining in a focus group or completing a questionnaire.
Patient and public involvement
Also known as PPI, involvement or public involvement, this is an active partnership between patients and the public and researchers in the research process. It is not people as subjects of research. Patient and public involvement in research is often defined as research done ‘with’ or ‘by’ people who use services rather than ‘to’, ‘about’ or ‘for’ them. This includes, for example, working with research funders to prioritise research, offering advice as members of a project steering group, commenting on and developing research materials, and undertaking interviews with research participants. When using the term ‘public’ we include patients, potential patients, carers and people who use health and social care services as well as people from organisations that represent people who use services.
Prioritisation
Rigorously examining potential topics for research to identify their importance and where the need for new evidence is greatest.
Public contributor
An umbrella term used to describe members of the public who take part in patient and public involvement activities. The definition of ‘public’ includes patients, potential patients, carers and people who use health and social care services as well as people from organisations that represent people who use services.
Public Partnerships
A term to collectively describe ways in which patients, service users, carers and members of the public work with researchers, and health and care professionals, in the creation and use of health and care research. Public partnerships encompass participation, involvement and engagement; they are all important in the process of creating and making use of high quality research. Each can take place in isolation, or in parallel. Experience, as well as research, has shown that they are mutually supportive in making research as relevant and impactful as possible. Use of the term Public Partnerships is not intended to replace, or make redundant, any existing terms or preferred ways of describing things.
Representative
One who is expected to speak on behalf of a larger group of people. If you’ve been asked to get involved in research as a representative of a particular group, you may want to think about how you can represent a wider range of people’s views, rather than just offering your own perspective.
Research
Essentially, the process of finding new knowledge that could lead to changes to treatments, policies or care. The definition used by the Department of Health is: “The attempt to derive generalisable new knowledge by addressing clearly defined questions with systematic and rigorous methods.”
Research Excellence Framework (REF)
The REF is the UK’s current system for assessing the quality of research in UK higher education institutions.
Research grant
Research grants are specific amounts of money given to researchers to carry out a particular piece of research. They might amount to millions of pounds for a major study about genetics for example, or a few hundred pounds for a local study about people’s experience of using a particular service. Usually, researchers have to write a research proposal and receive a positive peer review in order to receive a research grant.
Research methods
The ways researchers collect and analyse information. Research methods include interviews, questionnaires, diaries, clinical trials, experiments, analysing documents or statistics, and watching people’s behaviour.
Research proposal
This is usually an application form or set of papers that researchers complete to describe what research they want to do and how they want to do it. The proposal might address a specific research brief and also cover the aim of the research, what the research questions are, who will be involved (both as participants and in carrying out the research), the time-scale and the cost.
Researcher
Researchers are the people who do the research. They may carry out research for a living, and be based in a university, hospital or other institution, and/or they may be a service user or carer.
Reviewer
An individual with specific knowledge, experience and skills in a field of practice who undertakes an independent review of a grant application, commissioning brief or document for publication. The comments made by this independent ‘external reviewer’ are used to inform the funding decision or the preparation of a written document.
Service user
A service user is someone who uses or has used health and/or social care services because of illness or disability. Some people feel this term has negative connotations.
Social care
A range of services provided across different settings, usually in the community. These include: home care, day care and residential care for older people; residential care and fostering for children; support for parents of disabled children, for mental health service users, physically disabled people and people with learning difficulties; and support for carers.
Survivor researcher
Some people who have used health or social care services describe themselves as ‘survivors’, which they see as a more empowering term than ‘patient’ or ‘sufferer’. For example, some people who have used mental health services or who have experienced mental or emotional distress call themselves survivors of the psychiatric system. Some people who have recovered from cancer call themselves cancer survivors. If someone describes themselves as a survivor researcher, they are making a statement about the fact that they have used health or social care services as well as being a researcher.
Systematic review
A review of a clearly formulated question that uses systematic and explicit methods to identify, select, and critically appraise relevant research, and to collect and analyse data from the studies that are included in the review. Statistical methods (meta-analysis) may or may not be used to analyse and summarise the results of the included studies.
Annex B – Acknowledgements
We would like to thank and acknowledge the significant contributions made by
Steering Group
Adewale Adebajo
Shamaila Anwar
Eleni Chambers
Tina Coldham
Michelle Farr
Kay Gallacher
Mel Hughes
Lynn Laidlaw
Stan Papoulious
Madiha Sajid
Lise Sproson
Victoria Wilson
Evidence Research Team
Shoba Dawson
Angela Ruddock
Expert Reviewers
Sophie Staniszewska
Bella Starling
Project Team
Helen Baxter
Silvia Bortoli
Jodi Brown
Tina Coldham
Katie Howe
Candace Imison
Meerat Kaur
Annex C – Examples of NIHR and related good practice
Supporting inclusion in general
Good practice guidance
Shaping Our Lives is a non-profit making user-led organisation specialising in the inclusive involvement of Disabled people and people from other marginalised communities. Shaping Our Lives produces research and reports on involving diverse communities in policy, planning and delivery of services.
NIHR programmes, infrastructure and groups
-
- NIHR Underserved Communities programme
Building on the work of the INCLUDE guidance, in September 2020, the NIHR commissioned a cross-organisational programme to examine how to address the lack of inclusion for underserved groups in clinical research. The Underserved Communities programme aims to create a common understanding across the research landscape to encourage delivery of research where the need is greatest. It aims to prompt a cultural shift in attitudes and embed more inclusive ways of working. The programme’s current work includes:
-
-
- Design and development of a new, accessible research targeting tool
- Circulation and analysis of a survey to understand key barriers and enablers for engaging with research in underserved communities
- Promotion of pre-doctoral awards within Trusts or Academic Institutions which historically have fewer applications/successful applications.
-
NIHR INCLUDE framework, guidance and microsite.
The guidance, published in August 2020, aims to improve inclusion of underserved groups in clinical research. Work has continued to disseminate the guidance and embed it into the clinical research ecosystem. The microsite includes a selection of tools and resources including a free online course, as well as examples of good practice.
-
- A practical guide to inclusion in public involvement in health research: Lessons learnt from the Reaching Out programme (2021) The guide provides practical examples, lessons and tips for preparing for and delivering inclusive involvement.
- The NIHR resource for public involvement – Being Inclusive in Public Involvement in Health Research (2021) – a series of prompts for researchers and for those whose job it is to support public involvement in research (practitioners).
- The NIHR Research Design Service (RDS) has developed a toolkit to promote equality, diversity, and inclusion (EDI) in research. The toolkit helps RDS advisers and researchers to consider and embed EDI at each stage of their research project, from inception through to dissemination, implementation, and impact. NIHR Research Design Service’s EDI Toolkit – Launch webinar March 30th 2022
- NIHR Global Health Research: Community engagement and involvement
NIHR’s vision for Community Engagement and Involvement (CEI) is that all global health research is undertaken in collaboration with the communities who are most likely to be affected by the research outcomes. They want to enable those who are marginalised to have a meaningful voice both in the research funding process, as well as in the design, delivery and dissemination of research. Global Health Research – CEI
-
- NIHR School for Primary Care Research
A model of commissioning engagement and involvement of diverse, under-represented patient and public groups in research (i.e. whereby Voluntary, Community and Social Enterprise organisations are engaged to conduct PPI in partnership with a research organisation for a fee). Currently in the process of publishing an evaluation of this work but it has also been referred to in a blog.
Regional Initiatives
-
-
- Equality Impact Assessment toolkit developed by NIHR Applied Research Collaboration East Midlands. This toolkit consists of comprehensive training, a directory of useful resources, as well as ongoing advice and guidance.
-
-
-
- FOR Equity Focus On Research and Equity (FOR EQUITY) is a new web-based platform providing tools and resources to help make research evidence more relevant for action to reduce social and health inequalities. It is a joint NIHR School for Public Health Research and NIHR ARC North West Coast resource. It provides a revised version of the Health Inequalities Assessment Tool (HIAT), an inventory of existing guidance to support research teams in applying an equity lens in their studies and a library of resources.
-
The One Manchester Public & Community Forum brings together those who are already leading Public and Community Involvement and Engagement (PCIE) work around Greater Manchester. The aim is to maximise diversity and inclusion, enhance the value of ongoing work, and create shared actions to improve the health and well-being of people living in Greater Manchester. The forum brings together leaders (both staff and public) of public and community involvement and engagement from health and care organisations linking with the NIHR Applied Research Collaboration Greater Manchester (ARC GM) and Health Innovation Manchester. Partners include: Universities within Greater Manchester; NIHR infrastructure; health and social care providers; the GM Health and Social Care Partnership; voluntary, community and social enterprise sector.
-
-
- NIHR ARC West – A map of resources for co-producing research in health and social care This document provides a map of practical resources that can help when co-producing research in health and social care.
-
NIHR & Other Guidance for specific groups/topics
(listed alphabetically)
Care Homes
NIHR Research Ready Care Home Network
This network brings together care home staff, residents and researchers to facilitate the design and delivery of research. The aim is to improve the quality of life, treatments and care for all residents.
Communities
-
-
- Guidance developed by Greater Manchester CVO aims to provide community-based researchers with a framework to build trustworthiness into their research.
-
-
-
- Multiverse Lab – Multiverse Lab was made by Unfolding Theatre and jointly commissioned across the West’s regional research infrastructure. The project was an interactive online and in-person experience which aimed to identify the health and social care issues that matter most to local communities and answer the question “What is the health or social care breakthrough you hope to see in your lifetime?”. Multiverse Lab reached over 3,000 people across the region and the final report can be read here.
-
Demographic data collection
The Greater Manchester form aims to capture the demographic characteristics of those who participate, are engaged and involved in clinical research. The decision on which fields to include was informed by existing good practice and advice received from the EDI team within Manchester University NHS Foundation Trust (MFT, the host organisation for the NIHR Manchester BRC and CRF), public health monitoring (including the use of multiple indices of deprivation indicators), the Data Protection Act and the Equality and Human Rights Commission. The form was reviewed for accessibility by the HISG (including public contributors who are members of the HISG) and underwent a Data Protection Impact Assessment.
The form was anonymised, because it contains personal and sensitive information. In consultation with the Information Governance team of MFT, and The Christie (partner site for the NIHR Manchester CRF), the form was approved for use by the Information Governance Oversight Boards of each NHS Trust. If you intend to use the form, please consider how you will ensure the data protection and liaise with your relevant local teams and requirements.
Digital Inclusion
The Healthy Ageing Team in ARC GM are working with the GM Combined Authority to on a project on digital inclusion in older adults ARC GM | What factors have impacted on older people’s (75+) access/experience of digital public services during covid-19? (nihr.ac.uk).
Disabled people
Centre for Disability Studies Resources: The Centre for Disability Studies (CDS) is an interdisciplinary network of researchers from across the Social Sciences, Humanities and STEM subjects, carrying out research and teaching that helps achieve equality and social justice for disabled people, globally.
Dissemination
Training on more effective dissemination methods (notably visual and more accessible methods).
Drug and Alcohol problems
-
-
- Example of user-led research focussing on drug/ alcohol problems.
- Co-designing the implementation of research findings: Hussey, D., Trinder-Widdess, Z., Dee, C., Bagnall, D., Bojangles, T., & Kesten, J. M. (2019). Co-design of harm reduction materials for people who inject drugs to implement research findings. Harm Reduction Journal, 16(1), [36].
-
Ethnicity
Used by organisations delivering health research in higher education, local government, the NHS, the private sector and voluntary sector to assess their delivery of race equality in health research.
A tool to help trial teams consider which ethnic groups should be included in their trial, and what challenges they may face. The site has examples of how to use the Framework, along with other resources linked to involving different ethnic groups in trials.
-
-
- NIHR Applied Research Collaboration East Midlands
-
Has a research theme of Ethnicity and Health Equality, supports the Centre for Ethnic Health Research (see below) and is running a number of projects to improve the diversity of research.
-
-
- The Centre for Ethnic Health Research: Vision: “To reduce ethnic health inequalities”. Work with patients, the public, community and voluntary sectors, researchers, health and social care organisations and have a range of research resources including Black Asian and Minority Ethnic groups in health and social care research toolkit and resources to ensure ethnic diversity in COVID-19 research.
-
Gypsy, Roma Communities
Including the Missing Voices of Disabled People in Gypsy, Roma and Traveller (GRT) Communities
The voices of GRT Disabled people were identified as ‘missing’ by a project group led by the University of Worcester in partnership with Shaping Our Lives Service User and Disability Network, a user-led organisation. This report aimed to provide a platform for the narratives of Disabled people who live in GRT communities regarding experiences in accessing health and social care services.
Learning Disabilities
The Learning Disabilities Research Group shares ideas, learns from each other, and supports each other in doing inclusive research with people with learning disabilities.
Mental Health
Survivor Researcher Network (SRN) is a user-controlled independent network for all mental health service users and survivors with an interest in research.
Palliative care
New NIHR palliative care research partnerships
In January 2022, researchers from the palliative and end of life care research theme have successfully launched 3 unique Palliative Care Research Partnerships, funded by the NIHR. In all cases, the ambition of each palliative care partnership is to forge new collaborations including clinical, academic and lived experience experts, who will develop and submit competitive research proposals to the NIHR.
Payments guidance
NIHR guidance
Social Care Research
A training programme for members of the public to become co-researchers (Ulster University) Modules for service users and carers equip them to take on roles developing social care research, such as membership of research committees and grant awarding panels. These modules achieve credit towards the Postgraduate Certificate/Postgraduate Diploma/MSc in Development and Co-Production of Social Care Research.
Staff/Researcher Recruitment
“No more tick boxes” Roger Kline – NHS England (East of England)
Brings together research evidence to suggest what practical steps employers could (and should) take to improve staff recruitment and career progression. It focuses on the treatment of women, Disabled staff, and staff from Black and Minority Ethnic backgrounds.
Trauma
Trauma-informed practice in co-production resources: How to work with people in more supportive ways if they have experienced trauma.
Volunteer Registry
SHARE is an NHS Research Scotland initiative. It has been created to establish a register of people, aged 11 and over, interested in participating in health research. Participants agree to allow SHARE to use the coded data in their various secure NHS computer records to check whether they might be suitable for health research studies. All information is confidential; no-one can access this information without permission.
Annex D – References and Bibliography
Ayton, Darshini, Sandra Braaf, Angela Jones, Helena Teede, Madeleine Gardam, Heidi Bergmeier, and Helen Skouteris. 2021. ‘Barriers and Enablers to Consumer and Community Involvement in Research and Healthcare Improvement: Perspectives from Consumer Organisations, Health Services and Researchers in Melbourne, Australia’. Health & Social Care in the Community, July.
Banas, Jennifer R., Susan Magasi, Kim The, and David E. Victorson. 2019. ‘Recruiting and Retaining People With Disabilities for Qualitative Health Research: Challenges and Solutions’. Qualitative Health Research 29 (7): 1056–64.
Batty, G, G Humphrey, and B Meakin. 2022. ‘Tickboxes and Tokenism: Service User Involvement Report, 2022’. London: Shaping Our Lives.
Bearne, Lindsay, Tushna Vandrevala, Celayne Heaton-Heaton-Shrestha, Kristen Hanson, Nancy Delaney, and Sophia Quirke-MacFarlane. 2022. ‘How Do Members of the Public and People from Ethnically Diverse Communities Access and Use Health Research and Information? A Scoping Review and Qualitative Study’. Commissioned Research (unpublished). NIHR.
Beresford, Peter. 2013. Beyond the Usual Suspects. London: Shaping Our Lives.
Boaz, Annette, Robert Borst, Maarten Kok, and Alison O’Shea. 2021. ‘How Far Does an Emphasis on Stakeholder Engagement and Co-Production in Research Present a Threat to Academic Identity and Autonomy? A Prospective Study across Five European Countries’.
Bodicoat, Danielle H., Ash C. Routen, Andrew Willis, Winifred Ekezie, Clare Gillies, Claire Lawson, Thomas Yates, Francesco Zaccardi, Melanie J. Davies, and Kamlesh Khunti. 2021. ‘Promoting Inclusion in Clinical Trials-a Rapid Review of the Literature and Recommendations for Action’. Trials 22 (1): 880.
Boivin, Antoine, Tessa Richards, Laura Forsythe, Alexandre Grégoire, Audrey L’Espérance, Julia Abelson, and Kristin L. Carman. 2018. ‘Evaluating Patient and Public Involvement in Research’. BMJ 363 (December): k5147.
Bonetree, Clare, Susanne Martikke, and Sarah Wilkinson. 2022. ‘Good Evidence – A Guide to Help Community Organisations Produce Research That Gets Taken Seriously_compressed.Pdf’. Manchester: GMCVO.
Bonevski, Billie, Madeleine Randell, Chris Paul, Kathy Chapman, Laura Twyman, Jamie Bryant, Irena Brozek, and Clare Hughes. 2014. ‘Reaching the Hard-to-Reach: A Systematic Review of Strategies for Improving Health and Medical Research with Socially Disadvantaged Groups’. BMC Medical Research Methodology 14 (1): 42.
Boote, Jonathan D., Maureen Twiddy, Wendy Baird, Yvonne Birks, Clare Clarke, and Daniel Beever. 2015. ‘Supporting Public Involvement in Research Design and Grant Development: A Case Study of a Public Involvement Award Scheme Managed by a National Institute for Health Research (NIHR) Research Design Service (RDS)’. Health Expectations 18 (5): 1481–93.
Bower, Peter, Christos Grigoroglou, Laura Anselmi, Evangelos Kontopantelis, Matthew Sutton, Mark Ashworth, Philip Evans, Stephen Lock, Stephen Smye, and Kathryn Abel. 2020. ‘Is Health Research Undertaken Where the Burden of Disease Is Greatest? Observational Study of Geographical Inequalities in Recruitment to Research in England 2013–2018’. BMC Medicine 18 (1): 133.
Brett, Jo, Sophie Staniszewska, Carole Mockford, Sandra Herron‐Marx, John Hughes, Colin Tysall, and Rashida Suleman. 2012. ‘Mapping the Impact of Patient and Public Involvement on Health and Social Care Research: A Systematic Review’. Health Expectations : An International Journal of Public Participation in Health Care and Health Policy 17 (5): 637–50.
Broomfield, Katherine, Claire Craig, Sarah Smith, Georgina Jones, Simon Judge, and Karen Sage. 2021. ‘Creativity in Public Involvement: Supporting Authentic Collaboration and Inclusive Research with Seldom Heard Voices’. Research Involvement and Engagement 7 (1): 17.
Bryan, D, K Dunleavy, C Facer, O Forsdick, M Khan, K Malek, K Salt, and K Warren. 2018. Common Cause Research: Building Research Collaborations between Universities and Black and Minority Ethnic Communities. AHRC Connected Communities Programme : [distributor] AHRC Connected Communities Programme.
Chambers, D., L. Preston, Anna Topakas, Stevienna de Saille, Sarah Salway, Andrew Booth, Jeremy Dawson, and James Wilsdon. 2017. ‘Review of Diversity and Inclusion Literature and an Evaluation of Methodologies and Metrics Relating to Health Research’, September.
Chambers, Eleni, Clare Gardiner, Jill Thompson, and Jane Seymour. 2019. ‘Patient and Carer Involvement in Palliative Care Research: An Integrative Qualitative Evidence Synthesis Review’. Palliative Medicine 33 (8): 969–84.
Clark, Michael, Esther van Vliet, and Michelle Collins. 2021. ‘Reflections from the COVID‐19 Pandemic on Inequalities and Patient and Public Involvement and Engagement (PPIE) in Social Care, Health and Public Health Research’. Health Expectations : An International Journal of Public Participation in Health Care and Health Policy 24 (5): 1547–50.
Dawson, Shoba, Stephen M. Campbell, Sally J. Giles, Rebecca L. Morris, and Sudeh Cheraghi-Sohi. 2018. ‘Black and Minority Ethnic Group Involvement in Health and Social Care Research: A Systematic Review’. Health Expectations 21 (1): 3–22.
Farooqi, Azhar, Karan Jutlla, Raghu Raghavan, Andrew Wilson, Mohammud Shams Uddin, Carol Akroyd, Naina Patel, Pamela Peggy Campbell-Morris, and Aaisha Tasneem Farooqi. 2022. ‘Developing a Toolkit for Increasing the Participation of Black, Asian and Minority Ethnic Communities in Health and Social Care Research’. BMC Medical Research Methodology 22 (1): 17.
Farr, Michelle, Philippa Davies, Heidi Andrews, Darren Bagnall, Emer Brangan, and Rosemary Davies. 2021. ‘Co-Producing Knowledge in Health and Social Care Research: Reflections on the Challenges and Ways to Enable More Equal Relationships’. Humanities and Social Sciences Communications 8 (1): 1–7.
George, Sheba, Nelida Duran, and Keith Norris. 2014. ‘A Systematic Review of Barriers and Facilitators to Minority Research Participation Among African Americans, Latinos, Asian Americans, and Pacific Islanders’. American Journal of Public Health 104 (2): e16–31.
Hamlyn, Becky, Martin (TSMLP) Shanahan, Hannah Lewis, Ellen O’Donoghue, Tim Hanson, and Kevin Burchell. 2015. ‘Factors Affecting Public Engagement by Researchers’. London: Wellcome Trust.
Harrison, James D., Andrew D. Auerbach, Wendy Anderson, Maureen Fagan, Martha Carnie, Catherine Hanson, Jim Banta, et al. 2019. ‘Patient Stakeholder Engagement in Research: A Narrative Review to Describe Foundational Principles and Best Practice Activities’. Health Expectations: An International Journal of Public Participation in Health Care and Health Policy 22 (3): 307–16.
Heckert, Andrea, Laura P. Forsythe, Kristin L. Carman, Lori Frank, Rachel Hemphill, Emily A. Elstad, Laura Esmail, and Julie Kennedy Lesch. 2020. ‘Researchers, Patients, and Other Stakeholders’ Perspectives on Challenges to and Strategies for Engagement’. Research Involvement and Engagement 6 (1): 60.
Hickey, Gary, Katie Porter, Doreen Tembo, Una Rennard, Martha Tholanah, Peter Beresford, David Chandler, et al. 2022. ‘What Does “Good” Community and Public Engagement Look Like? Developing Relationships With Community Members in Global Health Research’. Frontiers in Public Health 9 (January): 776940.
HSRUK, Nuffield Trust, The Health Foundation, and The King’s Fund. 2022. ‘Improving Inclusion in Health and Care Research: Reflections and next Steps’. HSRUK.
Islam, Safina, Olivia Joseph, Atiha Chaudry, Davine Forde, Annie Keane, Cassie Wilson, Nasima Begum, et al. 2021. ‘“We Are Not Hard to Reach, but We May Find It Hard to Trust” …. Involving and Engaging “Seldom Listened to” Community Voices in Clinical Translational Health Research: A Social Innovation Approach’. Research Involvement and Engagement 7 (1): 46.
Kapadia, Dharmi, Jingwen Zhang, Sarah Salway, James Nazroo, Andrew Booth, Nazmy Villarroel-Williams, Laia Becares, and Anneez Esmail. 2022. ‘Ethnic Inequalities in Healthcare: A Rapid Evidence Review’. The NHS Race and Health Observatory.
Kleinman, Arthur, and Peter Benson. 2006. ‘Anthropology in the Clinic: The Problem of Cultural Competency and How to Fix It’. PLOS Medicine 3 (10): e294.
Laidlaw, Lynn. 2021. ‘Lynn Laidlaw: How Do We Bring Data and Its Outputs to Life?’.The BMJ.
Leslie, David, Anjali Mazumder, Aidan Peppin, Maria K. Wolters, and Alexa Hagerty. 2021. ‘Does “AI” Stand for Augmenting Inequality in the Era of Covid-19 Healthcare?’ BMJ 372 (March): n304.
Marmot, Michael, Jessica Allen, Tammy Boyce, Peter Goldblatt, and Joana Morrison. 2020. ‘Health Equity in England: The Marmot Review 10 Years On – The Health Foundation’. London: Health Foundation.
NIHR. 2021. ‘Best Research for Best Health: The Next Chapter’. NIHR.
Ocloo, Josephine, Sara Garfield, Bryony Dean Franklin, and Shoba Dawson. 2021. ‘Exploring the Theory, Barriers and Enablers for Patient and Public Involvement across Health, Social Care and Patient Safety: A Systematic Review of Reviews’. Health Research Policy and Systems 19 (1): 8.
Oudendammer, Willemijn M. den, Jacquelien Noordhoek, Rebecca Y. Abma-Schouten, Lieke van Houtum, Jacqueline E. W. Broerse, and Christine W. M. Dedding. 2019. ‘Patient Participation in Research Funding: An Overview of When, Why and How amongst Dutch Health Funds’. Research Involvement and Engagement 5 (November): 33.
Prinjha, Suman, Nasima Miah, Ebrahim Ali, and Andrew Farmer. 2020. ‘Including “Seldom Heard” Views in Research: Opportunities, Challenges and Recommendations from Focus Groups with British South Asian People with Type 2 Diabetes’. BMC Medical Research Methodology 20 (1): 157.
Russell, Jill, Nina Fudge, and Trish Greenhalgh. 2020. ‘The Impact of Public Involvement in Health Research: What Are We Measuring? Why Are We Measuring It? Should We Stop Measuring It?’ Research Involvement and Engagement 6: 63.
Smart, A. 2021. ‘Engaging Patients from Minority Ethnic Groups with Clinical Trials for Blood Cancer’. Commissioned Report. Blood Cancer UK. September 2021.
Smith, Christine. 2021. ‘Increasing Diversity on National Funding Committees: A Scoping Review’. Unpublished internal. NIHR Central Commissioning Facility.
Snape, D., J. Kirkham, N. Britten, K. Froggatt, F. Gradinger, F. Lobban, Jennie Popay, K. Wyatt, and Ann Jacoby. 2014. ‘Exploring Perceived Barriers, Drivers, Impacts and the Need for Evaluation of Public Involvement in Health and Social Care Research: A Modified Delphi Study’. BMJ Open 4 (6): e004943.
Staley, Kristina, Isabelle Abbey-Vital, and Claire Nolan. 2017. ‘The Impact of Involvement on Researchers: A Learning Experience’. Research Involvement and Engagement 3 (1): 20.
Staniszewska, Sophie, Amanda Blatch-Jones, Krysia DZiedzic, Richard Grant, Zoe Gray, Gary Hickey, Magdalena Skrybant, Richard Stephens, Sophie Werko, and Jane Whitehurst. 2021. ‘Patient and Public Involvement in the Work of NIHR Funding Committees: Key Messages Recommendations and Future Options’. Unpublished internal. NIHR Centre for Engagement and Dissemination.
Staniszewska, Sophie, Gary Hickey, Pippa Coutts, Ben Thurman, and Tina Coldham. 2022. ‘Co-Production: A Kind Revolution’. Research Involvement and Engagement 8 (1): 4.
Tembo, Doreen, Gary Hickey, Cristian Montenegro, David Chandler, Erica Nelson, Katie Porter, Lisa Dikomitis, et al. 2021. ‘Effective Engagement and Involvement with Community Stakeholders in the Co-Production of Global Health Research’. BMJ 372 (February): n178.
Tervalon, Melanie, and Jann Murray-Garcia. 1998. ‘Cultural Humility versus Cultural Competence: a critical distinction in defining physician training outcomes in multicultural education. Journal of Health Care for the Poor and Underserved 9 (2).
Turin, Tanvir Chowdhury, Nashit Chowdhury, Nahid Rumana, Mohammad A. A. Lasker, and Mahdi Qasqas. 2022. ‘Partnering with Organisations beyond Academia through Strategic Collaboration for Research and Mobilisation in Immigrant/Ethnic-Minority Communities’. BMJ Global Health 7 (3): e008201.
Waheed, Waquas, Adwoa Hughes-Morley, Adrine Woodham, Gill Allen, and Peter Bower. 2015. ‘Overcoming Barriers to Recruiting Ethnic Minorities to Mental Health Research: A Typology of Recruitment Strategies’. BMC Psychiatry 15 (1): 101.
Waite, Jacob, Fiona Poland, and Georgina Charlesworth. 2019. ‘Facilitators and Barriers to Co‐research by People with Dementia and Academic Researchers: Findings from a Qualitative Study’. Health Expectations : An International Journal of Public Participation in Health Care and Health Policy 22 (4): 761–71.
Wilkinson, Sarah, Clare Bonetree, and Hannah Berry. 2020. ‘The Value of Small Community-Led Equalities Research Projects’. Manchester: Ambition for Ageing.
–